GENERAL QUESTIONS
Q: Do I have to be Native American to get services here?
A: No, you do not. SNAHC is open to the community, there are no tribal or ethnic requirements to receive care here.
Q: What if I am from another County? Can I schedule an appointment with SNAHC?
A: Out-of-County Members who are changing counties due to a move or relocation must report this change to either their sending county or receiving county to begin the “Inter County Transfer”. The reporting county has 7 business days to initiate the transfer. If the beneficiary moves to another county and is still enrolled in a MCP (Managed Care Plan) in the county that they moved from, the beneficiary shall have continued access to emergency services and any other coverage the MCP authorizes out-of-network until the time that the ICT process is complete, and the beneficiary is disenrolled from the MCP.
Q: I don’t have a place to stay tonight. Can you give me a referral to an emergency shelter?
A: There are shelters available on a first come first serve basis in Sacramento County. 211 or www.211.org has a complete listing along with a list of qualifications.
Q: Do you have any bus passes?
A: We currently do not have a funding source to purchase bus passes for our patients.
Q: I would like to attend a SNAHC event. Where can I get more information?
A: A list of SNAHC-sponsored events and activities may be found in advance on the Community Calendar. Events and activities may change throughout the year.
Q: We would like SNAHC to host an information booth at our event.
A: Please forward all event sponsorship or attendance requests to the Outreach and Engagement Coordinator. Requests must be at least 30 days prior to the event.
Q: What is a Land Ackowledgement?
A: A land acknowledgement is a formal statement, a public recognition, of the Indigenous Peoples who have been dispossessed and displaced from their ancestral homelands and territories due to a variety of colonial and historical reasons. This statement acknowledges that an organization, a city, a park, or any other structure was built, and operates, on Indigenous Peoples’ ancestral homelands.
NATIVE PATIENTS
Q: What if I am Native American? How do I get assigned to SNAHC?
A: If an American Indian/Alaska Native patient or community member is enrolled in a managed care plan that we accept and wants to receive services at SNAHC they can initiate a provider change with our member services team. If a member has a managed care plan that we do not accept, you can call Health Care Options (1-800-430-4263) and change to a plan we accept. As an alternative to remaining enrolled in the managed care plan, we can assist members in filing for a Medi-Cal Exemption as their Indian Health Service Provider or you can call Health Care Options at 1-800-430-4263 before your appointment to apply for the waiver on your own. This would allow the patient to select straight Medi-Cal and remain outside of any specific plan.
Q: I am Native with no insurance; can I receive free services at SNAHC?
A: SNAHC does not currently have grant funds that would allow us to cover medical, dental, or behavioral health appointments/services for our native patients without insurance. We do, however, have a sliding scale based on income and family size with lower co-pays than our regular sliding scale. When you enroll as a member of SNAHC, we can put you on the native sliding scale (when you have provided proof of eligibility per Indian Health Service regulations), and also provide you with information on possible medical benefits like Medi-Cal or other public insurance programs.
Q: I have Medi-Cal/Medicare with another provider but I am Native and want Mental Health/SUD Services from SNAHC?
A: Native patients with “Straight” Medi-Cal or Medicare which means they are not assigned to a Managed Care Plan, or a Medicare Advantage Plan, are eligible for Mental Health/SUD. Native patients that have a managed care plan secondary to Medicare or have a Medicare Advantage plan will still require assignment to SNAHC if needing access to talk therapy with a Licensed Clinical Social Worker. If requesting services for SUD, an assignment change is not required.
Q: Where do I go to find out my Native roots? And how do I start?
A: Documenting Ancestry is our handy guide to discovering your Native heritage. Please also see this page of the Bureau of Indian Affairs.
Q: Where can I find other resources for the Native Community?
A: There are several Native serving organizations in our area. To learn more and find contact information, please review our Native Navigator.
PATIENT AND INSURANCE QUESTIONS
Q: What insurance plans do you accept?
We accept the following plans: Medicare, Medi-Cal, Anthem Blue Cross River City Medi-Cal, Molina Medi-Cal, Health Net River City Medi-Cal, and most private insurance plans. Please note, we only bill private insurance for our Native patients; these are typically considered out of network provider visits as we do not contract with private insurance companies. We are also a Family PACT and Every Woman Counts provider.
Q: I have Medi-Cal or Medicare, am I eligible for services at SNAHC?
A: SNAHC services are available to Medi-Cal and Medicare patients. Patients with “Straight” Medi-Cal or Medicare which means they are not assigned to a Managed Care Plan, or a Medicare Advantage Plan, are eligible for covered services.
Patients with Medi-Cal with Managed Care designations and Medicare Advantage Plans are assigned to specific Medical Groups or Independent Physician Associations (IPAs). Medical Groups and IPA’s have contracts with specific providers and assign patients to specific providers. SNAHC staff are required to verify eligibility and patient assignment prior to services being rendered.
Q: I have Medi-Cal and Medicare. Can I still be seen at SNAHC?
A: You can have both Medi-Cal and Medicare. Often referred to as Medi-Medi. The same rules apply to Medi-Cal Managed care and Medicare which often requires a provider assignment. Please call our office 916-341-0575 to determine eligibility or to change your provider and/or to become an assigned SNAHC patient.
Q: What is Medi-Cal Managed Care?
A: Sacramento is a Managed Care County. Medi-Cal Managed Care contracts for health care services through established networks of organized systems of care, which emphasize primary and preventive care. Managed care plans are a cost-effective use of health care resources that improve health care access and assure quality of care. These networks require referrals to specialty providers from your Primary Care Provider (PCP) and create access to a variety of providers that are organized to meet your specific health care needs.
SNAHC currently is contracted with Aetna, Anthem, Health Net, River City Medical Group, Imperial Health Plan, Nivano Health and Molina Medical Group.
Q: What is Medicare Advantage?
A: You can get your Medicare benefits through Original Medicare, or a Medicare Advantage Plan (like an HMO or PPO). If you have Original Medicare, the government pays for Medicare benefits when you get them. Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare. Medicare pays these companies to cover your Medicare benefits. If you join a Medicare Advantage Plan, the plan will provide all of your Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance) coverage.
SNAHC Currently Accepts multiple Medicare Advantage Plans, please call 916-341-0575 to determine eligibility.
Q: I have Medi-Cal but I don’t want to wait to be seen. Can I just pay cash?
A: Patients with Medi-Cal are not permitted to pay out of pocket even for out of county or out of network services as it violates Medi-Cal policy however, if a patient loses their Medi-Cal eligibility or is or becomes privately insured they are permitted to be seen via Sliding Fee Schedule or as private pay.
Q: What can I bring in for my proof of income? I am not working and do not have any income.
A: You can bring the following for proof of income: last year’s taxes (if filed), a benefits statement (if on unemployment, SSI, SSDI, SSA, SDI, GA, or Cal-Fresh), and FAFSA is okay if you are a student and applied for financial aid. If you do not have any of the acceptable documents, please contact Member Services at 916-341-0575 to determine the best way to provide proof of income.
Q: Why do I have to give you my social security number?
A: In addition to being a Patient-Centered Health Home, SNAHC is a Federally-Qualified Health Center (FQHC) and obtaining a patient’s social security number is one of the requirements for a complete Patient Record. If you cannot provide a social security number we cannot put you on the sliding scale, as this discount option is technically a federal benefit.
Q: What If SNAHC is not my assigned provider?
A: New Patients: If during the New Patient registration process, it is identified that a member is not assigned to SNAHC or a SNAHC provider, the Member Services Representative will offer to assist in conducting a PCP/PCD switch. If a member chooses to initiate during the registration, an appointment will be offered upon completion of the PCP/PCD switch and based on assignment date to SNAHC.
Established Patients: If at the time of eligibility verification, it is identified that the patient is not assigned to SNAHC or a SNAHC provider, the patient will be informed that a PCP/PCD switch will need to be completed, preferably with a Member Services Representative. If a situation arises in which a Member Services representative is not available, the front desk Patient Services representatives can initiate.
Q: What if I have other health coverage?
A: Patients with Other Health Coverage (OHC) or Private insurance through their employer or perhaps a parent: If at the time of eligibility verification, it is identified that the patient has (OHC) that we do not accept, they will be referred to Member Services to review their insurance, find out if the plan is active and conduct an OHC Removal if the plan is expired. During which time, the existing appointment will be canceled until insurance is cleared. In most cases, the “other Insurance” is contacted for a discontinuance of coverage letter. If a patient has active OHC, they will be referred to their in-network provider.
Q: How do I enroll in a Covered California Insurance Plan?
A: Please visit the Covered California website to locate a Certified Enrollment Counselor, if you are located in Sacramento you can call Sacramento Covered, (916) 414-8333 or visit their website https://www.sacramentocovered.org
Q: I want to know more about the Affordable Care Act (“Obamacare”). Can you tell me more?
A: Please visit the Covered California website to locate a Certified Enrollment Counselor.
Q: What do I choose for Geographic Managed Care (GMC) from Medi-Cal?
A: We will be accepting GMC’s with Anthem Blue Cross, Health Net (if part of River City Medical Group) and/or Molina at SNAHC. You can call a Health Care Options (HCO) Representative, toll free, at 1-800-430-4263, between 8:00 am to 5:00 pm, Monday-Friday to get more information.
Q: What does “other health coverage” mean?
A: Your insurance records indicate that you have or have had private insurance—you need to contact your former carrier or current social worker to try and remove it if it is not active.
Q: Do you have a Sliding Fee Scale for Payment?
A: No one will be denied access to services due to an inability to pay; there is a discounted/sliding fee schedule available based on family size and income.
Q: How does the referral process work at SNAHC?
A: Here is our 4-step process for how referral work at SNAHC.
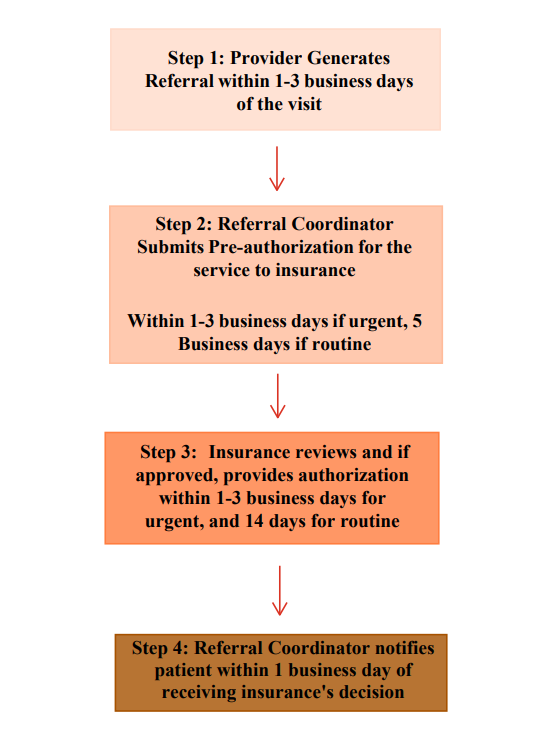
** The entire process may take up to 20 days **
Q: Why is my referral taking so long?
A: At the Sacramento Native American Health Center, we are always trying to give you the best care. We know it’s important for your referrals to be processed quickly and easily, and we understand that our referral process has recently been a source of frustration. In an effort to continuously improve. We have some exciting updates to help us serve you better.
Learn More »
Q: Why are Medicare telehealth services being changed?
A: There may be some updates to the telehealth services available to you. Due to absent Congressional action to extend telehealth flexibilities, Medicare patients will no longer be able to receive telehealth services for non-behavioral health care starting October 1, 2025. We will continue to communicate any changes that might affect you or your coverage as soon as we become aware of them, including if Congress officially decides that telehealth benefits for medical appointments will be continued.
Learn More »snahc.org
Still have questions? Call 916-341-0575 to speak with a patient services representative.
